I understand that people are terrified of dementia. Believe me, I get it. My mother died of Alzheimer’s. But I can’t wrap my head around the fact that advocacy for killing/suicide as the answer to the difficulties caused by the condition is becoming ubiquitous.
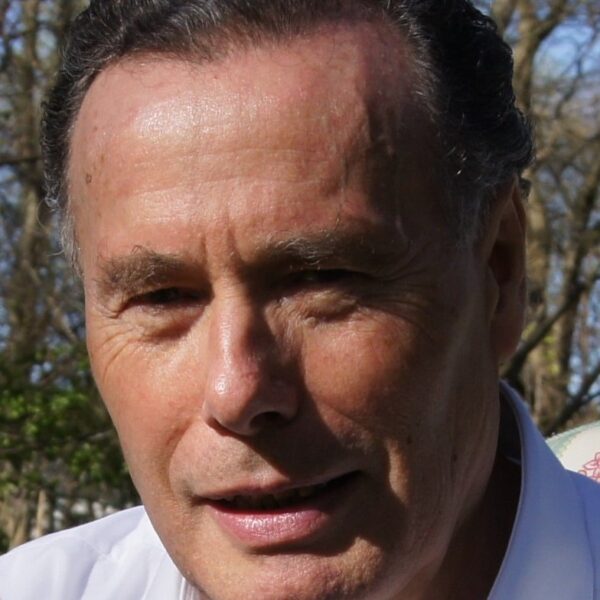
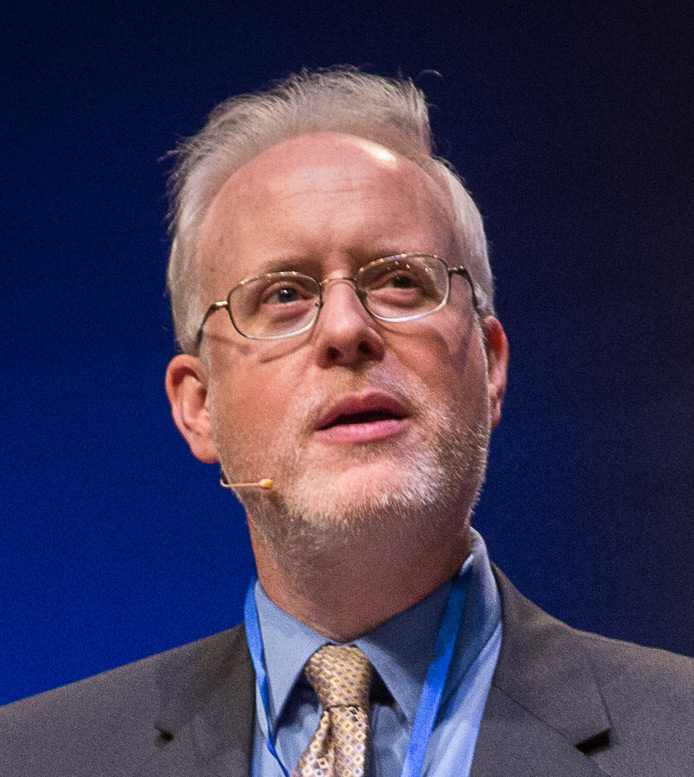
Noted bioethicist and lawyer Thaddeus Mason Pope has written an essay, to be published in an edited volume, on this very issue. It lists eleven ways people can “avoid late-stage dementia,” and almost all involve intentionally ending life.
Remember when we were told that advance medical directives are the key to not receiving life-extending treatment one does not want? They are, but that’s not good enough for Pope, because it doesn’t guarantee death:
This strategy is risky and uncertain. While patients with dementia can refuse antibiotics, they might never get an infection requiring antibiotics. In other words, advance directives for patients with dementia may be impotent because no triggering condition in their advance directive is ever satisfied. They may never need treatment they have refused. Consequently, traditional advance directives cannot reliably achieve the goals of patients seeking to avoid late-stage dementia.
Damned with Faint Praise
Not only that, but he barely touches on the kind of compassionate care that can be provided to dementia patients, such as hospice, properly delivered. He even damns hospice with faint praise:
While physical suffering is usually sufficiently addressed with hospice and palliative support, this long duration imposes a burden on the patient and their family. And it imposes a significant financial cost, as the patient typically has nursing and doula support.
Get it? This is an argument not to avoid suffering but to not be a “burden” and to put oneself out of loved ones’ misery.
Cross-posted at National Review.